Trauma refers to any deeply threatening or disturbing event, ranging from (witnessed or experienced) abuse to major disasters that overwhelms our coping capacity.
Understanding how trauma impacts us and why we respond in certain ways is key to healing.
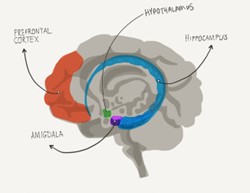
When we encounter acute stress, the part of our brain called hypothalamus stimulates secretion of stress hormones (e.g., cortisol) to help us deal with the immediate danger (Sherin and Nemeroff, 2011). You might know of the familiar “fight, flight, freeze” responses that reflect this survival mode (for more science, see Kozlowska et al., 2015).
Posttraumatic stress disorder (PTSD)
While several factors determine whether someone will develop PTSD, Normally after a traumatic event, anyone can experience:
- Intrusion symptoms: nightmares, flashbacks, intrusive thoughts
- Hyperarousal: insomnia, anger, easily startled, impulsivity
- Changes in cognitions or mood: can’t remember aspects of trauma; emotionally detached.
- Avoidance: of trauma reminders
When these symptoms persist, PTSD can develop and the brain can undergo several stress-induced changes.
- Hippocampus – for learning and memory
Enhanced cortisol secretion is known to impair hippocampus by damaging its neurons, and hindering its reformation. Studies have commonly found smaller hippocampus sizes in people with PTSD (Blum et al., 2019).
As the hippocampus plays an important role – in learning that danger is over and forming cohesive memories – if the person’s hippocampus gets suppressed during a fear response, then it’s likely they won’t remember some details of the traumatic event. When they re-encounter Trauma Triggers, there is also no information stored to tell them that danger is over.
- Amygdala – the danger detector
Brain studies have also revealed that in people with PTSD, there is pathological damage to their amygdala (Van Rooij et al., 2015). This relates to the amygdala being overstimulated by trauma, making it hyperactive irrespective of context.
Trauma survivors may be very alert to sensory reminders of their trauma, and get sent into a flashback followed by exaggerated responses – as though the trauma was happening in the here and now.
- Prefrontal cortex – the rational part of the brain
Survivors of sexual assault often blame themselves for why they “didn’t react” during the assault. But when the survival mode takes over, reflexes will trump reason (Bremner, 2006).
Connected to the amygdala is the medial prefrontal cortex, which has inhibitory control over the survival mode. However, decreased frontal cortex volumes have been found in people with PTSD (Koenigs and Grafman, 2009), which may account for symptom severity and why trauma survivors experience irrational fears that are difficult to overcome.
Several interactive networks between the prefrontal cortex and the amygdala have also been suggested by Yehuda and colleagues’ (2015). These explain the neurobiological workings of PTSD symptoms such as dysfunction in cognitive processing, arousal, and the processing of external information in relationship to oneself.
Complex trauma
Chronic exposure to trauma in childhood increases the likelihood of developing complex PTSD in adulthood. Herringa (2017) studied young people with PTSD and observed abnormal frontolimbic development including declining hippocampal volume, increasing amygdala reactivity, and declining amygdala-prefrontal coupling.
These may explain impaired emotion regulation and increased threat reactivity that paints a picture of the brain dominated by survival (rather than learning) mode as the young person ages. The resulting impairment could range across cognitive, emotional and social domains in their adult lives (Atkinson, 2013).
Treatment
Trauma significantly affects our brain in ways that can lead to lifelong problems. The best way to overcome these challenges is to seek trauma-focused therapies (sometimes in combination with medication)that have been shown to promote neurogenesis (Levy-Gigi et al., 2013).
Current gold standard psychotherapies include:
- Cognitive Processing Therapy (CPT)
- Prolonged Exposure (PE)
- Eye Movement Desensitization and Reprocessing (EMDR)
The Centre for Clinical psychology offers CPT to help people reprocess their beliefs and emotions impacted by trauma.
References:
Atkinson, J. (2013). Trauma-informed services and trauma-specific care for Indigenous Australian children (Closing the Gap Clearinghouse Resource 21). Canberra: Australian Institute of Health and Welfare.
Bremner, J. D. (2022). Traumatic stress: effects on the brain. Dialogues in clinical neuroscience.doi: 10.31887/DCNS.2006.8.4/jbremner
Herringa, R.J. Trauma, PTSD, and the Developing Brain. Current Psychiatry Reports, 19, 69 (2017). doi: 10.1007/s11920-017-0825-3
Levy-Gigi, E., Szabó, C., Kelemen, O., & Kéri, S. (2013). Association among clinical response, hippocampal volume, and FKBP5 gene expression in individuals with posttraumatic stress disorder receiving cognitive behavioral therapy. Biological psychiatry, 74(11), 793-800.
doi: 10.1016/j.biopsych.2013.05.017
Koenigs M, Grafman J. Posttraumatic Stress Disorder: The Role of Medial Prefrontal Cortex and Amygdala. The Neuroscientist. 2009, 15(5): 540-548. doi:10.1177/1073858409333072
Kozlowska K, Walker P, McLean L, Carrive P. Fear and the Defense Cascade: Clinical Implications and Management. Harvard Review of Psychiatry. 2015, 23(4):263-87. doi: 10.1097/HRP.0000000000000065
Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues in clinical neuroscience. 2011, 13(3): 263-78. doi: 10.31887/DCNS.2011.13.2/jsherin.
van Rooij SJ, Kennis M, Vink M, Geuze E. Predicting Treatment Outcome in PTSD: A Longitudinal Functional MRI Study on Trauma-Unrelated Emotional Processing. Neuropsychopharmacology. 2016 41(4): 1156-65. doi: 10.1038/npp.2015.257
Yehuda R, Hoge CW, McFarlane AC, Vermetten E, Lanius RA, Nievergelt CM, Hobfoll SE, Koenen KC, Neylan TC, Hyman SE. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015, 8 (1): 15057. doi: 10.1038/nrdp.2015.57